Everything you need to know
Contents
Here, we outline exactly what Patient Experience is, and why it is important, in short, digestible chunks. You can read our guide from top to bottom, or skip to a point that is most relevant for your needs.
While many organisations long to go back to pre-COVID times, the world is moving on and so is digital technology, especially in the healthcare industry.
Many healthcare providers and facilities are now fully embracing virtual and digital medical services that are paving the way to a new future of patient engagement.
As part of this transformation, the patient experience is expected to evolve.
To help you remain one step ahead of your patient needs, here are 4 key patient experience trends your healthcare facility will need to respond to in order to thrive in the post-COVID world:
1. Personalisation is now a priority
2. The utilisation of predictive analytics
3. Telehealth will be more prominent
4. Proactive patient care
Read more about these trends here.

Patients waiting in line at healthcare facilities face a huge sense of stress and worry. It’s not only inconvenient. It’s also often uncomfortable sitting around, watching the clock while being surrounded by other patients.
Here are the reasons why it’s essential to improve healthcare queuing:
1. Effective queueing prevents delays. With effective queuing, you can organise schedules, reduce wait times and hasten document processing to eliminate customer inconveniences and no-shows.
2. Better queue management saves time and costs. Efficient healthcare queueing ensures better patient flow management.
3. Improved healthcare queueing ensures quality service. When healthcare queueing is effectively managed, patient needs are more easily identified. As a result, you can provide them with more bespoke healthcare services – from the initial appointment to follow-up check-ups.
4. With proper queue management, you can take advantage of smart insights. Advanced healthcare queueing systems collect data and provide valuable insights that help you understand how to best enhance your services and meet evolving patient requirements.
5. Efficient queueing minimises the burden on your healthcare staff. By improving the queuing process, staff can focus on prioritising patient healthcare instead of spending their time and energy on preventing congestion and working on crowd control.
Read more here.
With health remaining a priority focus worldwide, making healthcare more accessible and convenient to patients has become increasingly important. As part of this, medical organisations are proactively looking for innovative ways to improve the overall patient experience, which is why they’re prioritising investment into suitable, patient-focused solutions.
Along with the advancements in technology and the evolving demands of people, delivering a rewarding experience in a convenient way continues to be a challenge for healthcare providers.
With the recent pandemic and evolving medical standards, NEXA embraced the opportunity to make a real difference for patients right across Western Australia through the introduction of a Smartphone App that allowed patients to take control of their own healthcare journey.
Read the Case Study here.
By working to understand your patient journey, you’re looking to put yourself in their shoes to gain insights into their experience with your healthcare facility from start to finish.
When you track your patient journey, you gain the opportunity to provide accountability, data accuracy and measurability to your organisation’s systems and processes. You’ll also experience benefits such as:
Improved competency within departments and services
Streamlined business reporting and auditing capabilities
Timely and effective communications with the patient
Improved administrative efficiency and management transparency
We live in a digital era where time is a very precious commodity. Optimising your patient journey through technology can dramatically improve patient wait times, save money and minimise risk within healthcare facilities. Find out more about the benefits of understanding your patient journey here.

Here are three trends that you can adopt as a healthcare provider to streamline your operations and provide a more positive patient experience – all of which can lead to better health outcomes and better business practise.
In many industries, transparency is not simply a suggestion, it’s a requirement. If you can find a way to make this information more available to your patients, it will go a long way towards improving their overall experience - and your reputation as a provider too.
Despite the evolution in digital technology over the years, many healthcare providers still manage their paperwork and operations manually. This leads to longer wait times, mismanaged queues, and delays in billing and payment processing, degrading the patient experience in the process.
Optimising the patient journey through automated technology can drastically reduce your patient wait times, save your resources, support your team and minimise mistakes within your healthcare facility.
Through the adoption of innovative and smart technology solutions, you can deliver better information, meet all deadlines, streamline your processes and ensure a positive patient experience every time. In doing so, you’ll safeguard your healthcare facility for the future, and ensure that you can remain adaptive to the ever-evolving needs of your patients over time. Read more about these trends here.

Having an effective hospital scheduling system in place can help decrease your patients’ waiting time, enable easy access to medical services and positively impact the quality of healthcare operations.
Therefore, enhancing the planning and scheduling procedures of your medical facility will play a vital role in the improvement of the hospital’s service quality that’s delivered to your patients.
Efficient scheduling plays a significant role in your healthcare team’s delivery of care and efficiencies, along with your ability to keep wait times to a minimum so that patient satisfaction levels remain high.
Here are 4 ways to make hospital scheduling work:
1. Send automated appointment reminders.These kinds of incremental improvements to your internal efficiencies and hospital scheduling systems will ensure your facility remains highly productive and continues to deliver the best experience for your patients. Read more about it here.
 By fostering a positive patient experience, a medical organisation can create better health outcomes and achieve higher patient retention rates, which is a win for everyone.
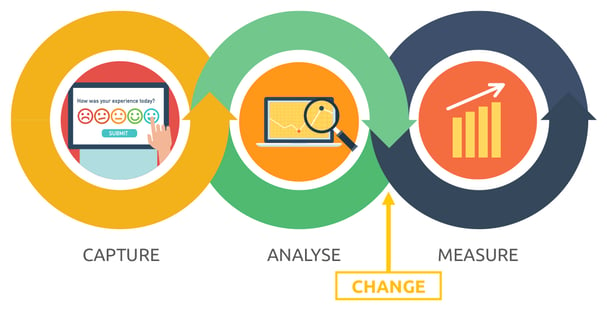
By fostering a positive patient experience, a medical organisation can create better health outcomes and achieve higher patient retention rates, which is a win for everyone.Healthcare facilities can utilise customer feedback to map the patient journey and assess their experience to:
For patients, capturing their feedback demonstrates that their input is appreciated, heard and valued. Internally, this feedback aids in establishing service KPIs and fostering a culture of innovation within your workforce.
Likewise, staff members who see your commitment to the continuous improvement and development of your facility can make them feel good about where they work and be more willing to contribute to its success. Find out more about streamlining your patient journey here.

Waiting times are one of the key quality metrics that can be used to define a positive or negative patient experience. While it can be complicated to communicate waiting times, the implications of not doing so can often be far worse. Let’s consider the negative impacts of not communicating wait times with patients:
By being aware of the risks involved with not communicating wait times, this can help your clinic find ways to communicate and even mitigate long wait times, rather than doing nothing and potentially damaging your reputation even further. Communication and education are key to overcoming these challenges and providing solutions for both parties. Read more here.
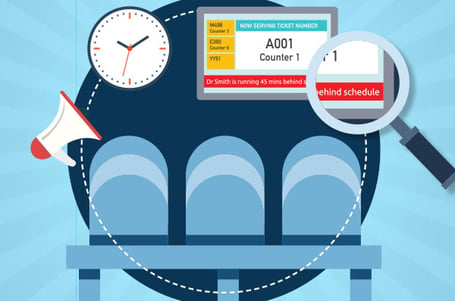
For many patients, the feeling of sitting in a waiting room and watching the minutes on the clock tick further and further past the time of their scheduled appointment is an all too familiar and frustrating one.
This can be detrimental to the operations of a healthcare provider, especially if it’s happening on a daily basis. People will then share their experiences with others and leave reviews, making the situation worse.
A patient’s feelings towards their healthcare provider can be highly dependent on the quality of their patient experience. In fact, a study published in the Journal of Medical Practice Management found that 96% of all patients attribute their frustration to a poor patient experience, rather than the quality or skill of their medical professional.
This is where NEXA’s Q-Flow platform comes in. Q-Flow is a digital tool that automatically organises your patients into a virtual queue while keeping them informed of their place in the queue in real-time.
Through the power of real-time notifications, you are providing a quality patient experience that leaves them feeling informed and valued. This will also clear up your waiting rooms and enable your staff to be more efficient. Read more here.

The waiting room, by very virtue of its name, has negative connotations for patients. For many, this is one of the first interactions they have with your clinic and whatever happens in the waiting room affects the general patient experience. The most pressing concern is always the long wait time.
At its heart, a good patient experience is comprised of removing friction (pain points) and creating an emotional connection. It takes around 12 positive experiences to make up for an unresolved negative one, so here are five steps to help you eliminate pain points from your waiting room:
1. Map the patient journey.
Patients today have high expectations of your service.
This means that every interaction is an opportunity to apply patient-centred design thinking, improve the quality of service and enhance the overall patient experience.
Communication plays a key role in this.
Let’s say we increase the level of communication between you, the patient, and the local healthcare clinic.
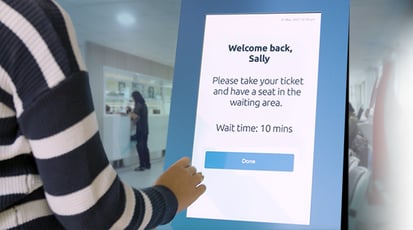
You have a scheduled appointment at 10:00am. You arrive at 9:40am to make sure that you are ready to see the healthcare provider on time. Then, you check-in for your appointment using the kiosk at the entrance to the facility.
Next, you are advised that, unfortunately, the healthcare provider will be approximately 30 minutes late this morning. However, they also tell you that if you provide your mobile number, you will be alerted when they are nearly ready to see you. Knowing this allows you to have some freedom around your wait time, making the experience more tolerable.
Effective patient communication is essential for delivering quality patient care and building good relationships. Clear, accurate, and timely communication maximises performance, improves patient outcomes and optimises service delivery. It also shows compassion and respect.
Read more about this here.
 One of the common misconceptions in the healthcare industry is that the patient experience should be focused predominantly on healthcare alone.
One of the common misconceptions in the healthcare industry is that the patient experience should be focused predominantly on healthcare alone.
The general public’s rising expectations of healthcare services means that every provider must take steps to improve their patient interactions.
The key to improving service design when it comes to patient satisfaction levels revolves a lot around your teams and the systems that support them. More than anything, providing a positive patient experience also empowers your staff to feel fulfilled and satisfied with their work as well.
Excellent service design ensures that all aspects of a patient’s healthcare journey make them feel valued and respected. It involves creating a positive environment for patients, staff, carers and volunteers through effective communication and the recognition of needs. Coupled with safe and high-quality care, service design minimises patient dissatisfaction and enables you to deliver a holistically pleasant experience – every time.
 13. Optimising your patient journey through technology
13. Optimising your patient journey through technologyWe live in a digital era where time is a very precious commodity.
Optimising your patient journey through technology can dramatically improve patient wait times, save money and minimise risk within healthcare facilities.
One example of this is the Gold Coast University Hospital, where they were able to decrease their patient check-in wait times from 20 minutes down to just 30 seconds after implementing innovative patient technology solutions.
With the continual growth and rising competition within the healthcare sector, ensuring a positive patient experience is now more critical than ever. Reviewing your patient journey regularly and investing in new solutions can lead to ongoing improvements in your processes, clinical treatments and more.
Read the Case Study here.
14. Improving communication between patients and health care providers
A lack of communication between healthcare providers and patients can be a major cause of frustration, especially in waiting rooms. The ‘line of visibility’ is a key component of service design because it separates all service touchpoints that are visible to the patient from those that are not. By applying service design methodology to address this gap in the patient experience, we can streamline processes and implement effective communication tools to empower the patients while they wait.
Learn how service design methodology can improve communication between patients and health care providers to improve the patient experience in this 40-minute webinar.

Improve the customer experience, with real data. NEXA is an Australian company that delivers innovative solutions to streamline the customer journey.
FOLLOW US ON LinkedIn
+61 (02) 8383 3800
sales@nexa.com.au
NEXA Group Pty Ltd
Level 6, 1 Newland Street,
Bondi Junction 2022
NSW Australia